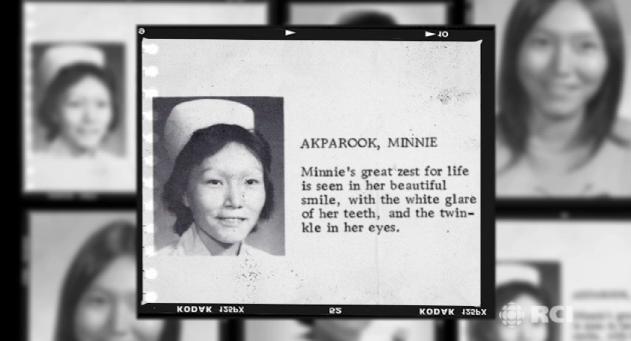
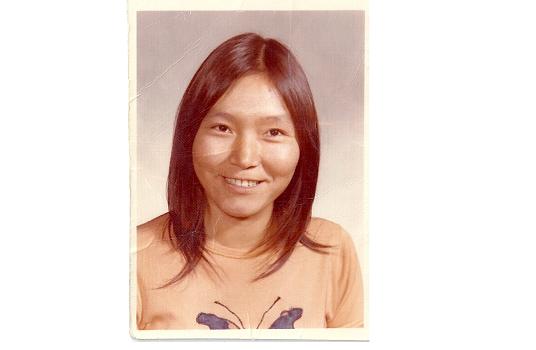
ARCTIC HEALTH SERIES – Bridging the Cultural Divide in Nursing: Minnie Akparook
 Nurses are on the frontlines of health care in Canada’s remote Arctic regions. Often working in isolated nursing stations, these health care professionals are part nurse, part emergency room doctor, part counsellor, part social worker and part mid-wife.
Nurses are on the frontlines of health care in Canada’s remote Arctic regions. Often working in isolated nursing stations, these health care professionals are part nurse, part emergency room doctor, part counsellor, part social worker and part mid-wife.
Most positions are filled by nurses from southern Canada who may not be familiar with local aboriginal languages or culture. This leads to high turnover and positions remaining vacant for long periods.
Many locals crave a stable work force staffed by aboriginal health care workers that understand northern culture and can deliver health services in local languages.
But despite this great need, there are still only a handful of such nurses practising in the Canadian Arctic. The road is often not easy for them. But once they begin working, they are able to bridge the cultural divide between southern medicine and holistic aboriginal culture.
To find out more, Eye on the Arctic sat down with Minnie Akparook, an Inuk nurse from Nunavik, Canada about the obstacles she overcame to start her career and the health challenges facing Canada’s Inuit population today.
On Becoming A Nurse
Where did you grow up?
I grew up in Great Whale, which is also known as Kuujjuarapik, in Northern Quebec.
What made you decide to go to school to become a nurse?
 There was a nurse that came from Great Britain in England. Her name was Miss Lutley. She was (in the North) for probably 20 years. We got close. When the federal government started sending students to Churchill, Manitoba, she wanted me to go. She got the Anglican minister behind her because my parents didn’t want to let me go. She finally said (to my parents) ‘I’ll pay you 25 dollars a month to let Minnie go to Churchill.’ My mother let me go for 25 dollars.
There was a nurse that came from Great Britain in England. Her name was Miss Lutley. She was (in the North) for probably 20 years. We got close. When the federal government started sending students to Churchill, Manitoba, she wanted me to go. She got the Anglican minister behind her because my parents didn’t want to let me go. She finally said (to my parents) ‘I’ll pay you 25 dollars a month to let Minnie go to Churchill.’ My mother let me go for 25 dollars.
What was it about nursing that attracted you?
Helping my own people. I have three brothers and three sisters. They all died. My mother could never have children that stayed alive but I saw (Miss Lutley) really helping her.
What was it like when you started nursing school?
I tried to go into nursing (in Winnipeg, Manitoba) as soon as I finished my high school grades. But people, I should say white people, were not ready for that. For me. So I quit nursing school when I had only six months to go. I didn’t heal from it for 20 years.
What made it so difficult?
I don’t remember there being anyone else there of a different colour or culture, so visibly different like me. It was the way people looked at you. You were let known 24-hours a day that you didn’t belong. But it wasn’t just in the school, it was everywhere. Even lunch counters in department stores. The Greensburo and Nashville sit-ins had been going on the United States but I was too much of a country bumpkin to realize it. So I just took it all in, internalized it all. I wasn’t political at all and didn’t even know what racism meant.
So you gave up on nursing?
 I never doubted that I’d complete it someday. But every time I actually thought about it, I would go back to the painful time. But when we moved to Timmons, Ontario from Yellowknife, I realized there was a nursing school there. I kept applying for the Registered Nurse program and they kept rejecting me. Finally when I applied for Registered Nurse’s Assistant they took me in and I transferred to the Registered Nurse class later.
I never doubted that I’d complete it someday. But every time I actually thought about it, I would go back to the painful time. But when we moved to Timmons, Ontario from Yellowknife, I realized there was a nursing school there. I kept applying for the Registered Nurse program and they kept rejecting me. Finally when I applied for Registered Nurse’s Assistant they took me in and I transferred to the Registered Nurse class later.
Puvirnituq is predominantly Inuit, what’s the reaction like now when you walk into a room?
I’m hoping they’re proud. It took a long time for me to get used to it and for them to get used to me.
On Health Care Challenges in the Arctic/Caring for an Arctic Population
How are health concerns different now than they were when you started practising 16 years ago?
From my point of view related to diabetes: the obesity. It rose. There’s no lack of food now. People don’t know which foods are good choices. White people have food eating schedules; breakfast, lunch and supper. Inuit don’t have that. They eat whenever and whenever there’s food available too.
And does that effect health even nowadays?
Especially for the person who is pre-diabetic and their body is struggling to control their blood sugar, yes. Very much.
What do you think are the main challenges of delivering health care in the North?
 It’s the great distances and the turn over (of health care workers). It’s really incredible.
It’s the great distances and the turn over (of health care workers). It’s really incredible.
Also, it’s very hard to translate medical terminology into Inuttitut.
The other challenge was that because the Inuit they see it macro not micro; so they don’t understand germs or they don’t understand your blood circulating in your body. It’s hard to explain to them that there’s something wrong with their body, with like diabetes, when they don’t feel sick.
Would it be helpful to have the different Arctic regions working more closely together so nurses in Northern Canada could talk to nurses in places like Greenland and the Sami territories in Northern Scandinavia and could learn from each others best practices?
I think that it is a good idea but only if there’s action behind whatever we’re doing. But if it just goes in the air like nothing happened, I don’t think so. Even within this community there’s disparity because we’re not together. Like with the municipal government, we should be more working together but I feel like we’re really not. But if there was action or a result it would be very helpful.
We’ve been hearing in the other Arctic regions as well that health systems are based on the southern way of doing things and doesn’t take into account Inuit culture. Have you seen this as a nurse?
It’s very frustrating on both sides. Nurses are expecting the reaction to be the same as in the South and it is not. The nurse gets frustrated because the Inuit sometimes does not follow the nurses instructions because maybe he didn’t understand or it’s not a normal thing to do in Inuit culture. But the nurse wants them to do it so they can be healthy again. They’re working against each other.
Way back down south before they hire them, there needs to be cultural orientation. There needs to be someone saying: ‘This is what you’re going to encounter. These are the people.’ From someone who knows what they’re talking about.
What do you think needs to be done to have more nurses, actually from the communities, working in the North?
People like you trying to get the story out that we need them. Teachers and people who are in charge of education really pushing, pushing, pushing. It’s a really good experience to be a nurse. You get more than you give. You’re saving lives.
Do you consider yourself a role model?
No and I don’t want to be. Really. I feel like I don’t qualify.

This article was contributed by Eilís Quinn, Radio Canada International as part of the Eye on the Arctic ARCTIC HEALTH SERIES – Part I: OUR SYSTEMS. This article was published during National Nursing Week, 2011.



